Surgeons in Boston achieved a breakthrough by transplanting a genetically engineered kidney in a 62-year-old male last weekend, in what is considered a first-of-its-kind procedure. If successful, the transplant could provide new hope for millions of kidney patients worldwide.
Read more:
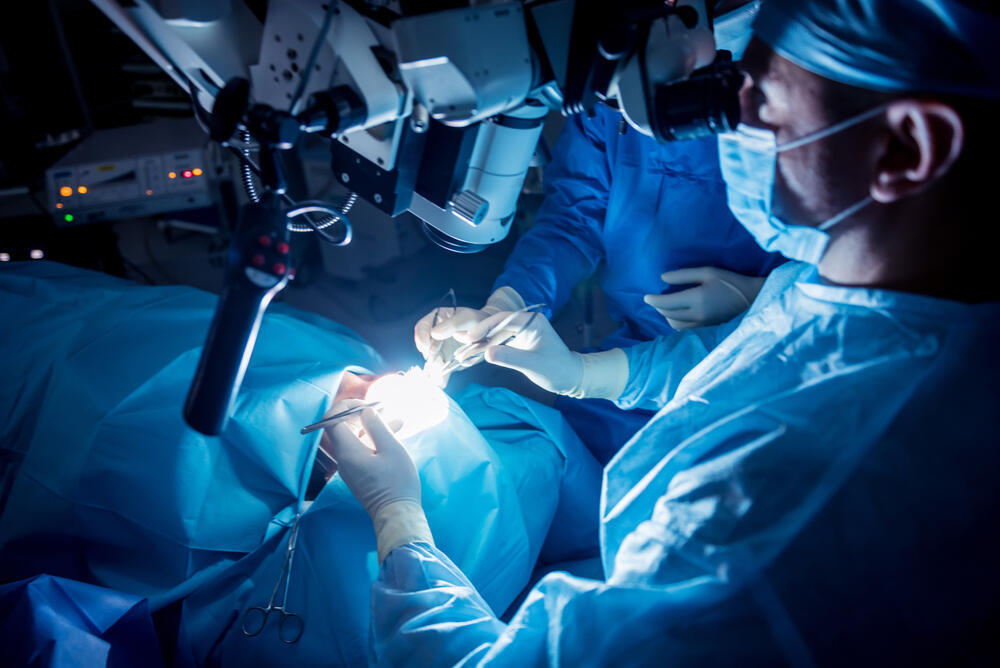
The surgery lasted four hours, and according to doctors at Massachusetts General Hospital, the signs are promising: the new kidney began producing urine shortly after the surgery last weekend, and the patient's condition continues to improve. He has already stopped dialysis, walks around the hospital corridors, and may be discharged soon.
The transplanted kidney came from a genetically engineered pig donated by the biotech company eGenesis, which removed three genes involved in organ rejection and added seven human genes to improve human compatibility. Pigs carry retroviruses that can infect humans, and eGenesis disabled these pathogens.
"Our hope is that this transplant approach will offer a lifeline to millions of patients worldwide who are suffering from kidney failure," said Dr. Tatsuo Kawai, the hospital's director for clinical transplant tolerance, in the hospital statement. More than 800,000 Americans suffer from kidney failure and require regular dialysis. Over 100,000 are on the waiting list for a kidney transplant. Additionally, tens of millions of Americans suffer from chronic kidney disease.
"I saw it not only as a way to help me, but a way to provide hope for the thousands of people who need a transplant to survive," Slayman said in a statement released by the hospital.
The patient, Richard Slayman, a transportation supervisor in Massachusetts, has been suffering from diabetes and high blood pressure for many years and has been treated at Massachusetts General Hospital for over a decade. He has been dependent on dialysis for seven years, and after renewing dialysis treatment last year, he experienced severe complications with his blood vessels and required rehospitalization.
The transplant "represents a potential breakthrough in solving one of the more intractable problems in our field, that being unequal access for ethnic minority patients to the opportunity for kidney transplants due to the extreme donor organ shortage and other system-based barriers," said Dr. Winfred Williams, the kidney specialist treating Slayman.
Dr. Williams suggested the experimental procedure to Sleiman, and after deliberation, he agreed. "I saw it not only as a way to help myself but as a way to provide hope to thousands of people in need of a transplant to survive," Sleiman said in a hospital statement. "He looks like a new person, it's amazing," said Dr. Williams.
Slayman got a human kidney transplant after being on dialysis for seven years, according to the hospital. But his transplanted kidney showed signs of failure after about five years, forcing Slayman to resume dialysis last May. He's since been suffering serious complications.
"When my transplanted kidney began failing in 2023, I again trusted my care team at MGH to meet my goals of not just improving my quality of life but extending it," Slayman said in the hospital's statement, adding the doctors explained the "pros and cons of this procedure."