A new therapeutic approach developed by the Weizmann Institute could spell a new hope in the battle against the COVID-19 pandemic.
Though vaccines may be steering the world toward a post-pandemic normal, the constant mutation of the pathogen (known as SARS-CoV-2) necessitates the development of far more effective drugs.
In a new study published on the online journal "Nature Microbiology" — researchers from Israel's Weizmann Institute of Science, France's Pasteur Institute and the U.S. National Institutes of Health (NIH) — offer a novel therapeutic approach to combating the virus.
Rather than targeting the viral protein responsible for the virus entering the cell, the team of researchers addressed the protein on our cells’ membrane that enables the process.
Using an advanced self-developed artificial evolution method, researchers generated a molecular “super cork” that physically jams this “entry port,” thus preventing the virus from attaching itself onto the cell and entering it.
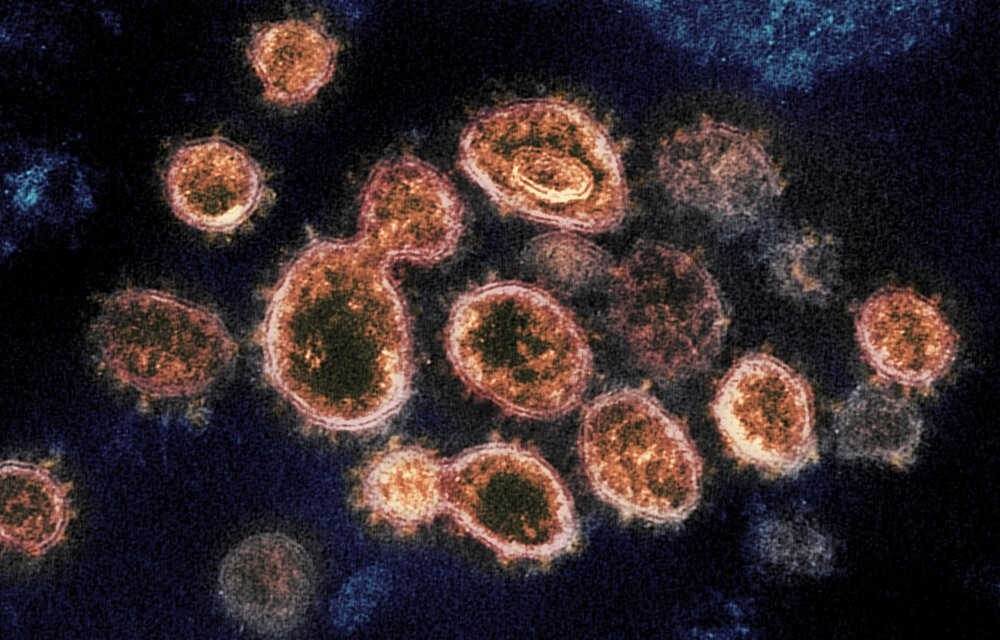
Most potential therapies and present vaccines for SARS-CoV-2 target the “spike protein” found on the virus’ outer envelope. This protein, however, is prone to mutations that erode the efficacy of these treatments.
“Since the virus is constantly evolving we have, instead, focused on the non-evolving human receptor called ACE2 that acts as the entry site for the virus,” said Prof. Gideon Schreiber of Weizmann’s Biomolecular Sciences Department who supervised the new study.
This approach is not susceptible to new emerging virus variants which is one of the main challenges in fighting the pandemic.
ACE2, attached to the membrane of lung epithelial cells and other tissues, is an enzyme important for regulating blood pressure. Therefore, as tempting as it may be to simply block this receptor to prevent the entry of SARS-CoV-2, any such strategy must not interfere with ACE2’s function.
Schreiber, whose lab specializes in studying interactions between proteins, set out to develop a small protein molecule that could bind to ACE2 better than SARS-CoV-2 does but without affecting the receptor’s enzymatic activity.
The researchers, led by Dr. Jiří Zahradník, a postdoctoral fellow researcher in Schreiber’s group, began by identifying SARS-CoV-2’s binding domain, the relatively short sequence of building blocks within the larger spike protein that physically binds to ACE2.
Using the virus’ own receptor binding domain as a weapon against it, Zahradník performed several rounds of “evolution-in-a-test-tube,” developed in Schreiber’s lab, on a genetically engineered strain of baker’s yeast.
Since yeast can be easily manipulated, Zahradník was able to rapidly scan millions of different mutations that accumulated in the course of this artificial evolution, a process that imitates natural evolution at a much faster pace.
Ultimately, the goal was to find a small molecule that would be significantly “stickier” than the original viral version.
During this scanning process, Schreiber’s team supplied strong evidence in favor of the hypothesis that SARS-CoV-2 becomes more contagious when mutations improve its fit to ACE2.
The researchers found that already after the first round of selection, the lab-made variants with tighter binding capabilities to ACE2 mimicked the mutations present in the binding domains of the most contagious SARS-CoV-2 strains that had occurred by means of natural evolution, such as the British variant (Alpha), the South African variant (Beta) and the Brazilian variant (Gamma).
3 View gallery


An elderly man receiving the third jab of the COVID vaccine due to the increased virality of the Delta variant
(Photo: Moti Kimchi)
Surprisingly, the now widespread Indian (Delta) variant relies on a different trick which makes it more transmissible — by partially evading detection by the immune system.
Eventually, Zahradník isolated a small protein fragment with a binding capability 1,000 times stronger than that of the original binding domain from which it evolved.
This “super cork” not only fit ACE2 like a glove but was also found by Maya Shemesh and Shir Marciano, Ph.D. students in Schreiber’s lab, to conserve the enzymatic activity of ACE2 — just as the researchers had intended.
Furthermore, owing to the strong binding, very low concentrations of the newly engineered molecule were needed to achieve the desired blocking effect.
To develop a potential method for administering the molecule as a drug, Schreiber and his team collaborated with Prof. Yinon Rudich of Weizmann’s Earth and Planetary Sciences Department. Together with Dr. Ira Marton and Dr. Chunlin Li, they created an aerosol-based spray that would allow the developed molecule to be administered to patients by inhalation.
So far, NIH researchers have tested the formulation in hamsters infected with SARS-CoV-2. Preliminary results indicate that this treatment significantly reduces the disease's symptoms.
More preclinical studies are slated to take place at the NIH in the near future.