Daily financial worries which involve paying bills and even the ability to put healthy food on the table are not just psychological concerns. A large-scale study has found that socioeconomic distress, particularly financial stress and food insecurity, is linked to accelerated aging of the heart, sometimes at a level similar to or greater than well-known medical risk factors such as high blood pressure and diabetes.
The study, recently published in the journal Mayo Clinic Proceedings, analyzed data from more than 280,000 adults who sought care at the Mayo Clinic between 2018 and 2023. Participants completed questionnaires on socioeconomic factors in their lives and underwent electrocardiograms as part of their medical care.
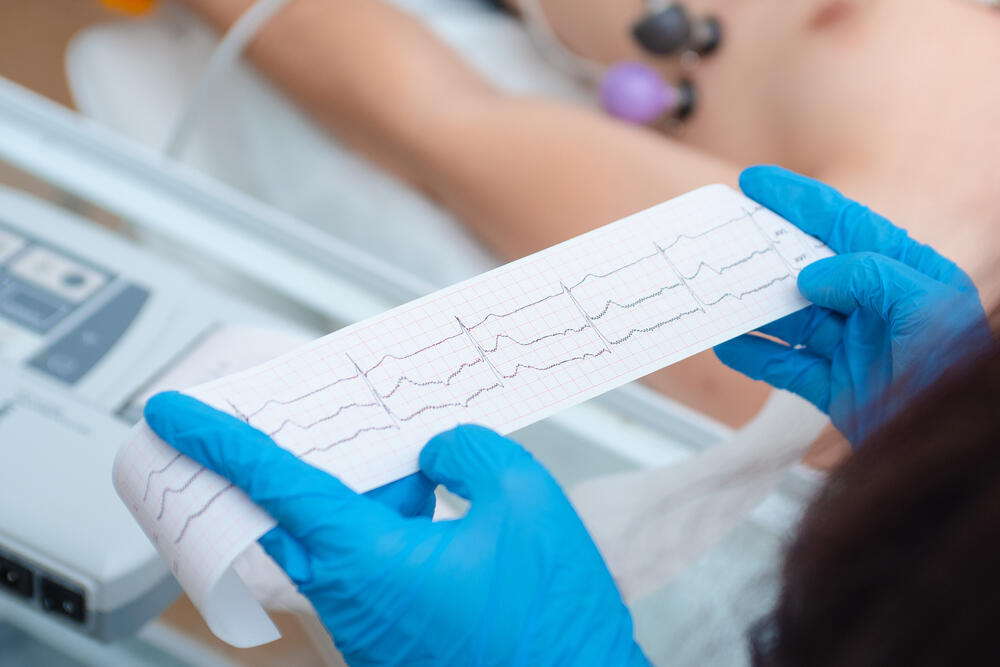
2 View gallery


Financial stress and food insecurity may cause the heart to 'age' faster
(Photo: Shutterstock)
Dr. Elias Hellou, a senior cardiologist in the catheterization unit at Emek Medical Center, stated that evidence has been steadily accumulating in recent years, showing that social factors have a direct impact on heart health and the pace of cardiac aging. Social hardship, financial insecurity, food insecurity and even mobility difficulties, he explained, are not merely background conditions but factors that actively influence a person’s “heart age.”
“Just as physical activity, healthy nutrition and social support benefit the heart, prolonged distress works in the opposite direction,” Hellou said. “The brain and mental state directly affect the cardiovascular system and can speed up cardiac aging or, in other situations, slow it down.”
Dr. Hellou noted that existing studies, including the current one, are largely based on large observational data sets that show a clear link between living conditions and heart aging. “The next step,” he said, “is to move from observational research to interventional studies and examine whether actively improving social, economic and nutritional conditions can actually slow heart aging and improve patients’ long-term health.”
 Dr. Elias HellouPhoto: Courtesy
Dr. Elias HellouPhoto: CourtesyWhat does ‘heart age’ mean?
Rather than focusing solely on whether a person had heart disease, researchers used technology that estimates “heart age” based on an electrocardiogram analyzed with artificial intelligence, known as AI-ECG. They compared the estimated heart age with a person’s chronological age to determine whether the heart appeared older than expected.
The main conclusion was clear. Among all the life factors examined, two stood out most strongly in their association with accelerated heart aging: financial stress and food insecurity, defined as uncertainty about access to sufficient and nutritious food.
Researchers also found that socioeconomic factors made a significant contribution to predicting heart aging, in some cases exceeding that of established medical risk factors.
The study also examined mortality over an average follow-up period of about two years. Certain forms of socioeconomic distress, especially financial strain related to limited resources, were significantly associated with a higher risk of death, even after adjusting for medical risk factors.
2 View gallery
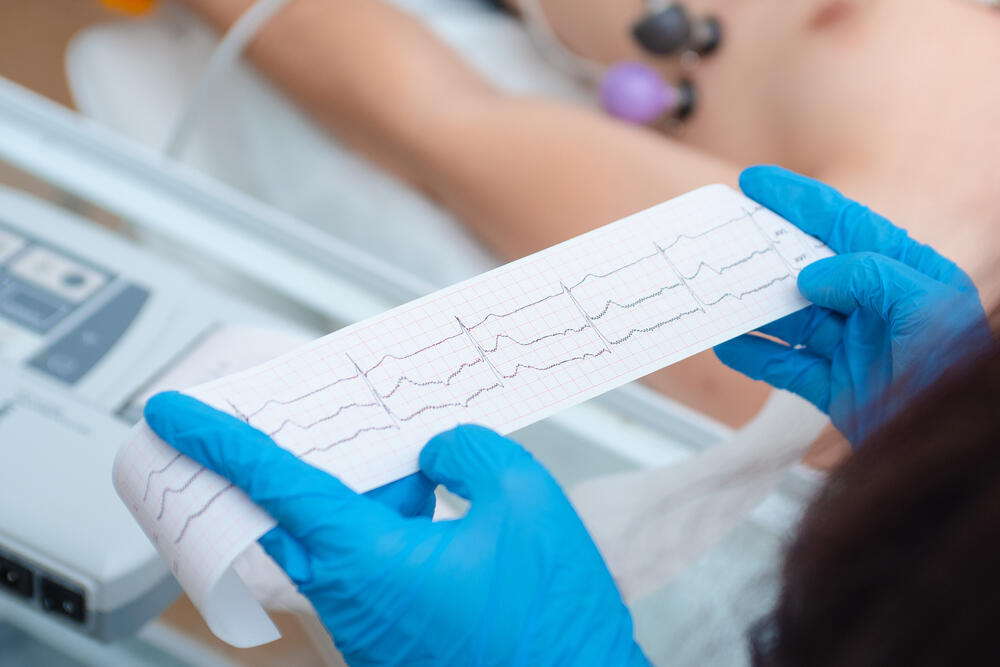
An electrocardiogram analyzed using AI allowed researchers to estimate 'heart age' and assess the impact of financial stress on the heart
(Photo: Shutterstock)
Dr. Leana Wen, an emergency physician and associate professor at George Washington University, told CNN that "heart aging refers to structural and functional changes in the cardiovascular system that increase the risk of heart disease. These include stiffening of blood vessels, changes in heart muscle function and impaired ability of the cardiovascular system to respond to exertion."
"Chronic stress can accelerate these processes", Wen said. "Stress hormones like cortisol and adrenaline affect blood pressure, heart rate, inflammation and metabolism," she added.
"When these systems are activated repeatedly over long periods, they can contribute to wear and tear on the heart and blood vessels. Over time, that cumulative effect may resemble what we see with aging or long-standing medical conditions."
Why does financial stress affect the heart so strongly?
Wen emphasized that financial stress differs from short-term stress, such as a temporary workload or a tight deadline. "Financial strain is often chronic and ongoing. It can involve persistent worries about bills, housing stability, medical expenses, debt or support of family members." That kind of stress is "difficult to escape", she said.
"Because money affects so many aspects of daily life, financial stress has a cumulative effect. It may disrupt sleep, limit access to healthy food or medical care, and reduce opportunities for exercise or rest. All these factors compound one another and can amplify cardiovascular risk over time", Wen said.
It does not mean that people experiencing economic hardship are "doomed to poor heart health", said Wen. Risk is influenced by many factors, and there are still meaningful actions individuals and clinicians can take to reduce harm."
The key message emerging from both the study and Dr. Wen's expert commentary is that alongside medical tests, medications and management of traditional risk factors, living conditions themselves must be addressed. Ongoing stress, financial insecurity and daily hardship are not merely background issues but part of the overall health picture, with a tangible impact on heart health.
The foundation of heart health remains the same: regular physical activity, a balanced heart-healthy diet, maintaining a healthy weight, avoiding smoking, controlling blood pressure, cholesterol and blood sugar, and undergoing routine checkups, since many risk factors develop without early symptoms.
Above all, Wen stressed, chronic stress should be treated as a health risk in its own right. Adequate sleep, mindfulness practices and stronger social connections can help soften the body’s stress response and provide additional support for heart health.
Wen said financial stress should be considered in medical decision-making just like other risk factors, such as family history or lifestyle. “This does not mean clinicians need to solve financial problems,” she told CNN, “but they can help connect patients to resources, adjust treatment plans to reduce financial burden, and be mindful of how stress may affect adherence to medications or lifestyle recommendations.”


