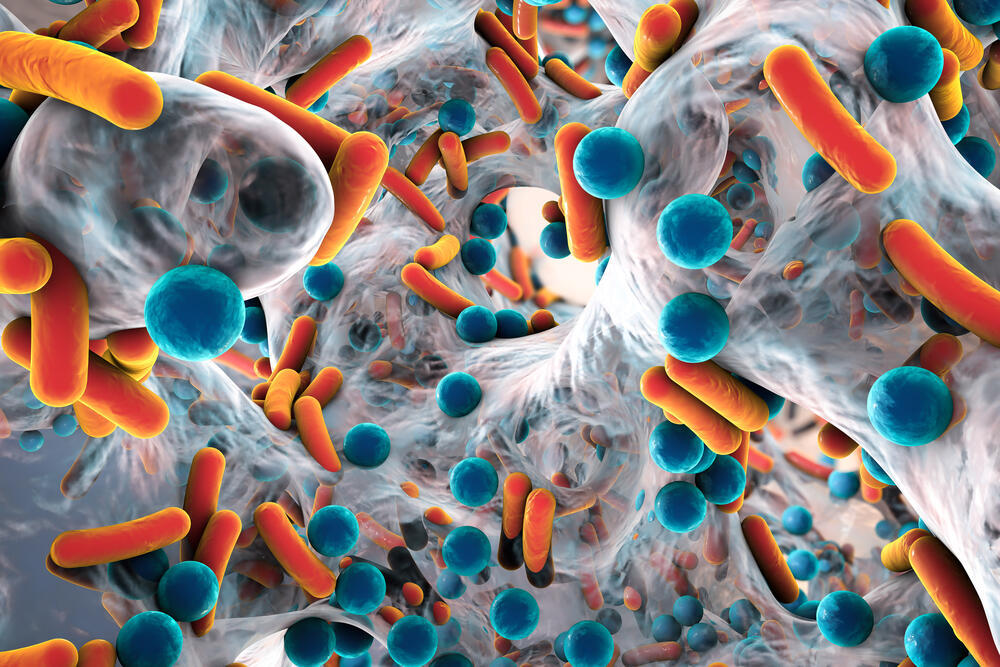
A new international study conducted over two decades and involving over 100 countries suggests there is a link between air pollution and resistance to antibiotics. While the study didn’t find the exact cause, evidence suggests that fine particulate air pollution with a size of PM2.5 may contain antibiotic-resistant bacteria or resistant genes that could directly enter human beings through inhalation or consumption.
More stories:
Resistance isn't futile
Antibiotic resistance is one of the most significant threats in the medical world and is estimated to cause the death of up to 1.3 million people annually. The main contributing factor to resistance is the overuse of antibiotics, primarily for viral illnesses.
The phenomenon of antibiotic resistance is also well evident in Israel: currently, "Helicobacter pylori," a bacterium that causes stomach ulcers, has a high tolerance to antibiotics. The treatment plan against the bacterium now includes the simultaneous use of four antibiotics.
Antibiotic resistance is increasing and is noticeable in Israel in sexually transmitted diseases, as well as in various pathogenic bacteria that are prevalent mainly in intensive care units.
Even without the observed resistance, air pollution poses a major environmental risk to public health. Prolonged exposure to air pollution is linked to chronic conditions such as heart disease, asthma, and lung cancer, which reduce life expectancy.
Short-term exposure is also hazardous and can lead to coughing, wheezing, asthma attacks, and a high rate of doctor visits and hospitalizations.
Reducing air pollution could, according to the researchers, help decrease antibiotic resistance, reduce mortality rates, and alleviate economic costs stemming from antibiotic-resistant infections.
The study’s head author, Prof. Hong Chen from Zhejiang University in China, said antibiotic resistance and air pollution are each in their own right among the greatest threats to global health."
“Until now, we didn’t have a clear picture of the possible links between the two, but this work suggests the benefits of controlling air pollution could be twofold: not only will it reduce the harmful effects of poor air quality, it could also play a major role in combatting the rise and spread of antibiotic-resistant bacteria,” he added.
Although air is recognized as a fast route for the spread of antibiotic resistance, data on the various pathways through which antibiotic-resistant genes are transported via air pollution is limited.
“Antibiotic resistance and air pollution are each in their own right among the greatest threats to global health."
Potential pathways include hospitals, farms, and water treatment facilities that release particles carrying antibiotic-resistant genes into the air, which then spread over long distances.
Until today, limited data existed on the extent of the impact of PM2.5 air pollution - composed of tiny particles 30 times smaller than a human hair - on global antibiotic resistance. PM2.5 sources include traffic emissions, industrial processes, domestic coal, and wood burning.
Evidence suggests that 7.3 billion people worldwide are directly exposed to unsafe annual averages of PM2.5 levels.
The researchers created an extensive database to investigate whether PM2.5 is a key driver of global antibiotic resistance, using data from 116 countries from 2000 to 2018. Their sources included the World Health Organization (WHO), the European Environment Agency, and the World Bank.
The findings indicate a rise in antibiotic resistance with PM2.5 levels, where each 10% increase in air pollution is associated with a 1.1% increase in antibiotic resistance.
The connection has strengthened over time, with changes in PM2.5 levels leading to larger increases in antibiotic resistance in recent years. The analysis suggests that antibiotic resistance due to air pollution was linked to 480,000 premature deaths in 2018.
A model of possible future scenarios indicates that without changes in current air pollution policies, global antibiotic resistance levels could increase by 17% by 2050. Annual deaths related to antibiotic resistance could rise to around 840,000.
The researchers also noted their study’s limitations, including data gaps in certain countries that could affect the results of the final analysis. The study was observational, so a direct cause-and-effect link between air pollution and antibiotic resistance was not established, the authors added.
Researchers called for further studies to focus on confirming this link and understanding the underlying mechanisms of how air pollution affects antibiotic treatment.
Results of antibiotic Overreliance
While antibiotics save lives, their excessive use is deadly. Experts warned about the widespread use of antibiotics leading to bacterial resistance over a decade ago. As it stands, many infectious diseases already lack effective treatment due to this resistance.
According to WHO data from 2017, the highest antibiotic consumption worldwide was recorded in the Far East, where each child receives an average of 3.5 antibiotic treatments per year.
In the United States and Eastern Europe, children receive around 1-1.5 antibiotic treatments per year on average, while in Scandinavian countries, a reduction in the use of antibiotics is most significant, with children receiving 0.5 or even fewer treatments per year.
In Israel, antibiotic consumption rates are similar to those in the United States, averaging between 1 to 1.5 antibiotic treatments per child per year.
This excessive usage leads to the emergence of deadly antibiotic-resistant bacteria. A report published seven years ago indicated that among European countries, Israel ranked second in the prevalence of the aggressive MRSA bacteria, which is resistant to most types of antibiotics globally.
Additional resistance to antibiotics has been noted concerning other aggressive bacteria like E. coli, Salmonella, and Klebsiella. The increasing resistance of bacteria to antibiotics holds severe consequences: in the near future, mild infections or minor wounds might become untreatable with antibiotics, potentially leading to death.
The World Health Organization blames the development of resistant bacteria on the widespread unnecessary use of antibiotics and the excessive use of potent antibiotics even for mild infections. Additionally, pharmaceutical companies are not developing new antibiotics, leading the organization to predict mortality rates from simple infections will rise.
One of these resistant bacteria is MRSA, which causes the death of 19,000 people in the United States each year. A similar number of deaths from MRSA infections is also reported in Europe every year.
Even the once-easily-treated E. coli bacterium has developed resistant strains, rendering simple antibiotics ineffective in over half of the cases.
Israel is worried
How do bacteria develop resistance to antibiotics? Thanks to their ability to adapt to their environment. One of the ways bacteria change is by producing an enzyme called beta-lactamase. This enzyme breaks down the "beta-lactam" ring found in many antibiotics such as penicillin, cephalosporins, carbapenems, and monobactams.
This process prevents antibiotics from inhibiting the formation of the bacterial cell wall, allowing the bacteria to continue growing, enter the bloodstream, and in severe cases, even lead to death.
In another mechanism, resistant bacteria prevent antibiotics from entering the cell by altering the composition of the bacterium and its interaction with the cell it infects. Other bacteria actively remove the antibiotic from the cell before it can affect the resistant bacteria, or they expel the antibiotic out of the cell that they've infected.
Resistant bacteria emerge through mutation: due to repeated exposure to antibiotics, some bacteria alter their DNA and create a drug-resistant strain of themselves. This strain continues to grow and spread.
A report by Israel’s State Comptroller warned about the widespread use of antibiotics in Israel nearly a decade ago, leading to severe infections. The report noted that infections in Israel cause around 5,000 deaths per year, with 25% to 75% of them being preventable.