Brain metastases originating from colon cancer are becoming more common—resulting from a combination of improved treatments, prolonged patient survival, and biological changes that enable cancer to adapt to the brain’s environment. However, despite this increase, there are often no effective treatment options for these metastases.
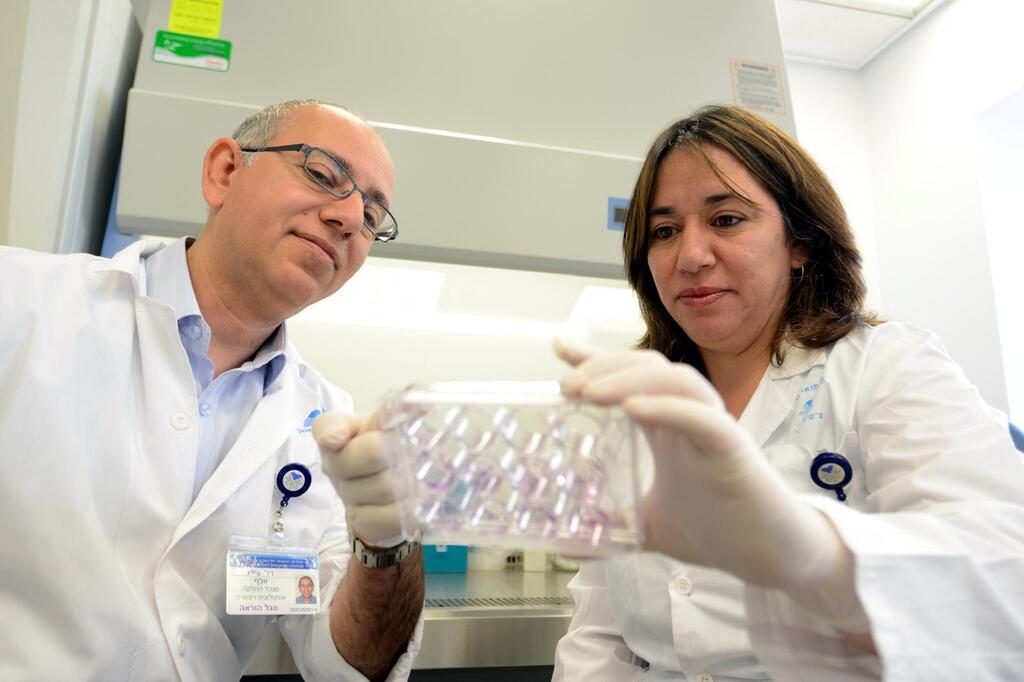
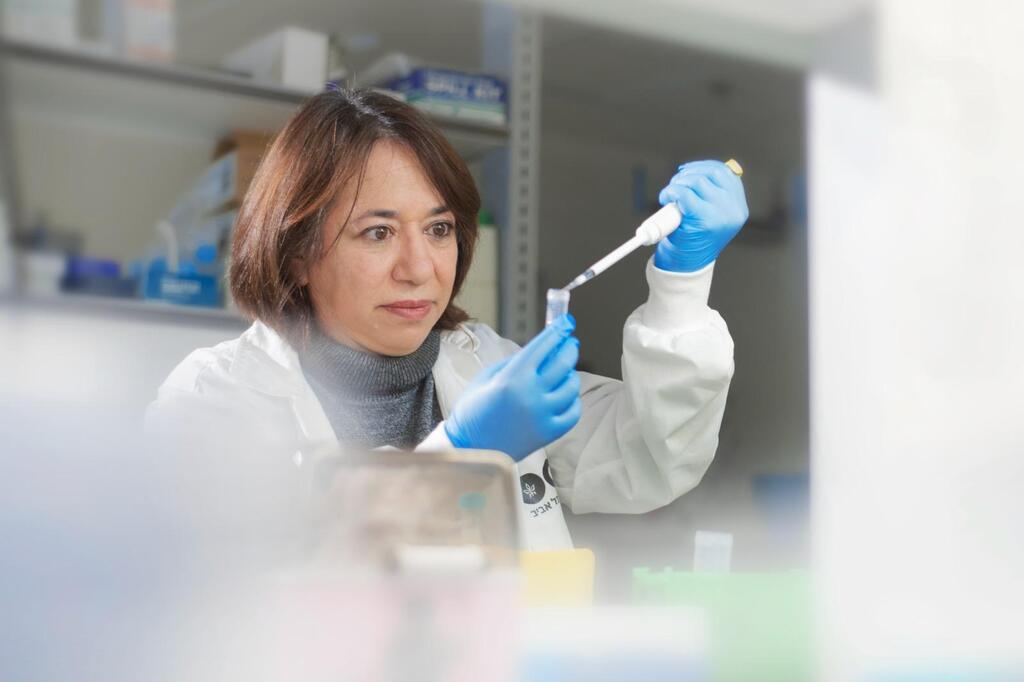
A new study conducted by researchers at the oncology department of Sourasky Medical Center, led by Prof. Ido Wolf, Dr. Tami Rubinek, and Dr. Inbal Greenberg, offers a surprising new insight: cancer cells change their nature when they infiltrate the brain, and their survival secret lies in a single protein—IRS2.
The study, published in the prestigious journal Neuro-Oncology, analyzed a genetic database of more than 35,000 colon cancer samples. The researchers compared primary tumors to metastases in various organs. In brain metastases—but not in the liver or lungs—they found increased expression of IRS2, a protein that transmits cellular signals related to growth and metabolism, primarily through insulin and IGF-1 receptors.
"Brain: A hostile environment for cancer cells"
"The brain is a hostile environment for cancer cells: less oxygen, less nutrition, and numerous barriers," explains Dr. Rubinek, lead researcher in the oncology research lab at Sourasky Medical Center. "We discovered that the IRS2 protein helps cancer cells cope with these extreme conditions. It activates the beta-catenin pathway and strengthens the mitochondria, enabling the cells to make better use of the limited resources available."
To further investigate the role of IRS2, the researchers examined its effects in various biological models: cell cultures exposed to environments simulating brain, liver, and lung tissues; mice injected with cells with or without IRS2 expression; and ex vivo systems designed to mimic the response of living environments. "In every model, we saw that cells with IRS2 survived and proliferated much better specifically in the brain environment," says Dr. Greenberg, who conducted her PhD research in the oncology research lab as part of her MD/PhD studies at Tel Aviv University. "The advantage these cells had almost disappeared when they moved to other environments, proving that this is a mechanism unique to brain metastases."
A new experimental treatment
To see if this survival mechanism could be disrupted, the researchers combined treatment with an experimental drug called NT219, which irreversibly inhibits IRS2, along with classic chemotherapy (5FU). In mice, this combination not only significantly slowed the development of metastases but also extended survival. "The chemotherapy alone didn’t work. Only when we added NT219 did we see a significant response," says Dr. Greenberg. "In mice that received the combination, the metastases were smaller, fewer, and in some cases, didn’t develop at all. This provides a strong foundation for an innovative treatment."
Get the Ynetnews app on your smartphone: Google Play: https://bit.ly/4eJ37pE | Apple App Store: https://bit.ly/3ZL7iNv
In addition to its direct impact, this mechanism plays a role in preventing drug resistance. In chemotherapy treatments, cancer cells often activate the beta-catenin pathway, which grants them resistance. However, when IRS2 is blocked, this pathway isn’t activated, leaving the cells vulnerable. "This isn’t just a new treatment—it’s a mechanism that restores the effectiveness of old treatments that no longer worked," emphasizes Dr. Greenberg.
When will this treatment reach patients?
NT219 has already completed the first phase of clinical trials in humans, where its safety was confirmed. Now, a more advanced clinical trial is planned to test its effectiveness against brain metastases. "If we see in humans what we saw in mice, this will be a breakthrough," says Prof. Wolf, head of the oncology department at Sourasky Medical Center. "There’s potential for accelerated approval, especially for patients in critical condition with no other treatment options."
Preventing metastases before they start
The next goal is not just to treat brain metastases but to prevent them. According to the researchers, if patients with increased IRS2 expression are identified early, targeted treatment could potentially prevent the development of metastases. "This is a realistic goal," says Dr. Rubinek. "It’s not just about curing—it’s about stopping the process before it begins."
This discovery also expands our understanding of how cancer cells survive in general. "Cells that manage to survive in the brain can also survive in other challenging organs," says Prof. Wolf. "IRS2 teaches us a broad principle about how cancer cells adapt to hostile conditions—so inhibiting it could improve treatment for metastases in the liver, lungs, and abdomen as well. This isn’t just a localized solution—it’s a new approach to treating resistant cancers."
Challenges ahead
However, the researchers stress that even with this promising discovery, there are many challenges ahead: differences between patients, variability among metastases, the risk of impacting healthy cells, and the biological complexity of the brain. "Not all cancer cells behave the same way," says Dr. Rubinek. "We’ll need tools to identify who is suitable for the treatment, and we’ll need to monitor its long-term safety—especially when dealing with a sensitive environment like the brain."