About a year ago, the tissue bank at Sheba Medical Center, Israel’s national bank for bones and tendons, received an urgent call from a pediatric orthopedic surgeon. He described a year-and-a-half-old baby hospitalized at the Safra Children’s Hospital at Sheba after being diagnosed with cancer in the femur, the largest and strongest bone in the human body.
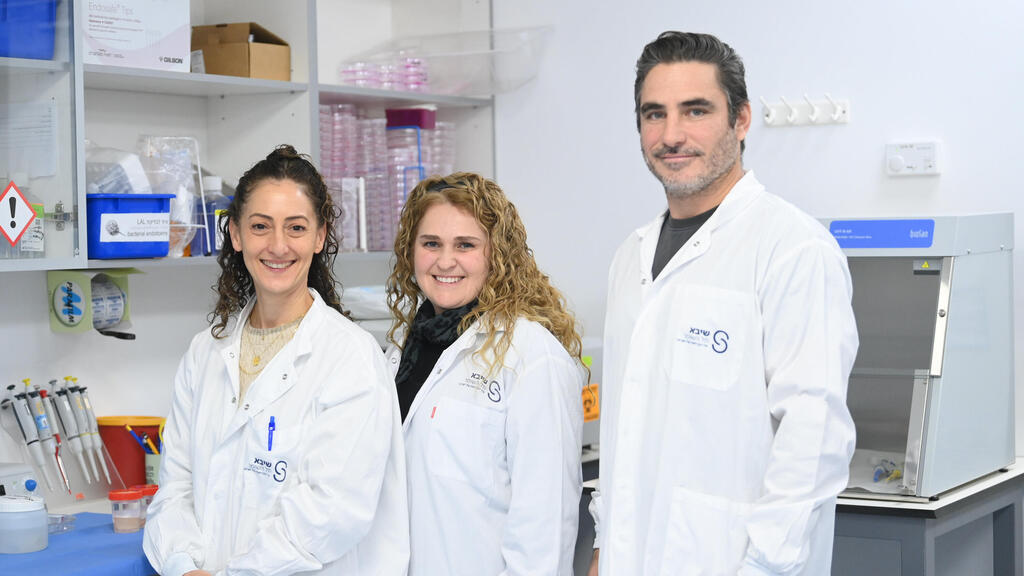
“He told me that the option to save the child’s life was amputation and asked whether we could offer a less radical alternative,” said Dr. Ayelet Di Segni, director of Sheba’s tissue bank. “Because we have the expertise to find biological solutions, we took on the challenge.”
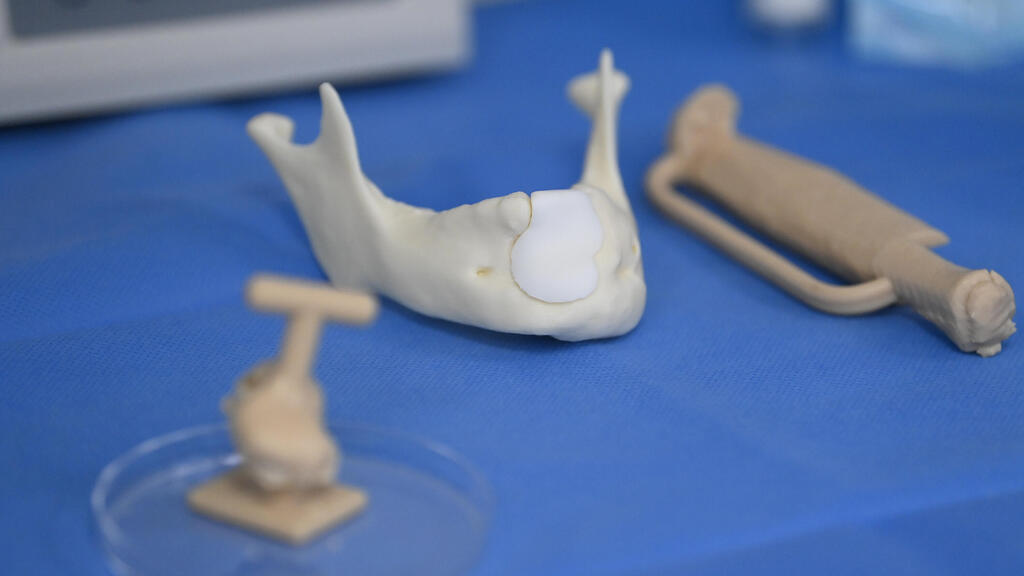
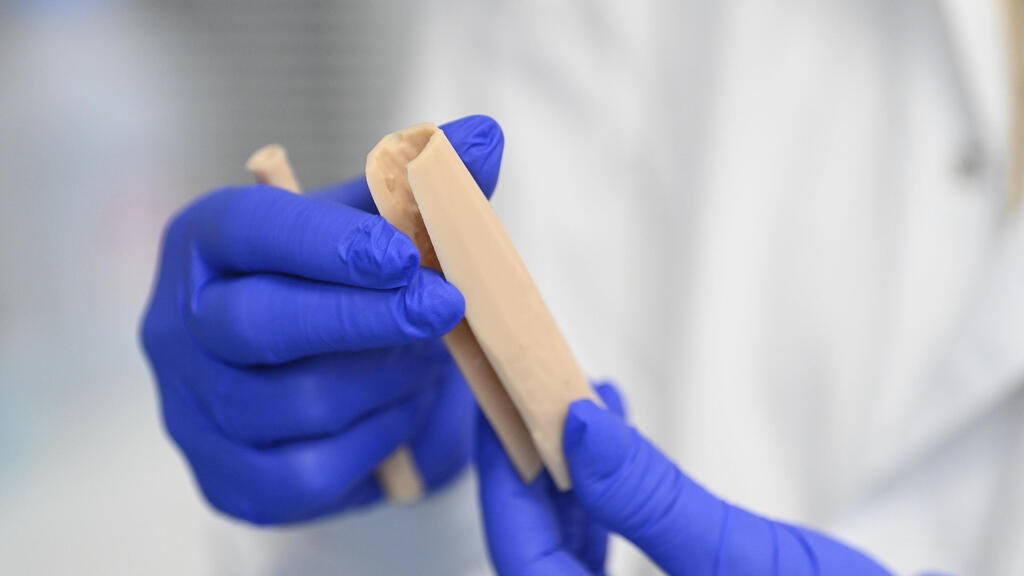
Working with Sheba’s 3D laboratory, the team used imaging scans to create an exact model of the affected area. They took a donated bone from the bank, drilled a channel through it and inserted living bone taken from the child’s own body.
“In a kind of ‘sausage in a bun’ structure, we created a precisely fitted replacement implant for the cavity left after the tumor was removed,” Di Segni said. “Blood vessels nourished the bone, allowing it to integrate and transform from dead bone into living bone.”
Footage and images from the procedure later showed the scale of the effort behind the scenes.
The anatomical tissue bank stores human tissue for transplantation, including skin, tendons, bones, corneas and heart valves. Di Segni said the bank was reestablished in 2022 after extensive study of leading centers abroad, shifting tissue processing from an operating room product to a laboratory-based process under strict guidelines and quality standards.
The bank has two main divisions. One focuses on cellular therapy, producing, growing and storing skin grafts, including for patients with severe burns. The other preserves tissues donated from deceased donors.
“In the skin graft division, we work in clean rooms,” Di Segni said. “Moving between rooms requires changing into sterile clothing, and entering the core area means wearing fully sterile suits that resemble space suits.”
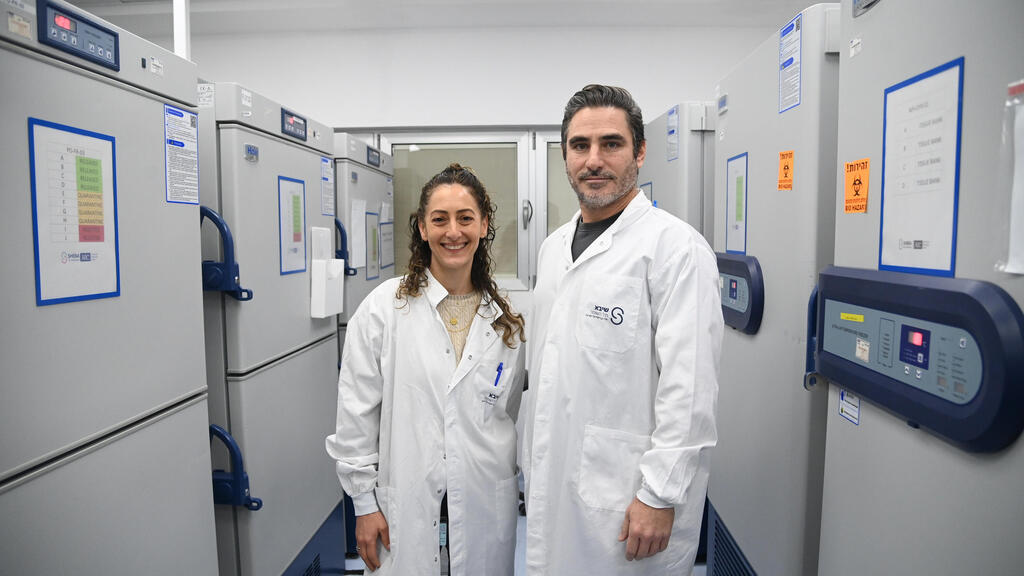
The laboratory includes research and development areas alongside large storage rooms with tightly monitored freezers at various temperatures and nitrogen tanks used to preserve different tissues. Alarms alert staff to any deviation.
“This is probably the most closely monitored warehouse of human spare parts you can imagine,” she said.
Heart valves are stored in liquid nitrogen at minus 196 degrees Celsius, said Alina Levy, a medical technologist who oversees heart valve processing at Sheba.
“When a donated heart arrives, I remove the valves, assess their quality, sterilize them and then freeze them,” Levy said. The valves are used exclusively for children with congenital heart defects because they grow with the child, sparing them repeated replacement surgeries.
Another clean room is dedicated to maximizing the use of donated bone, said Dr. Ron Borstein, deputy director of the tissue laboratory and a former veterinarian.
“We have three machines here, each with increasing levels of processing,” Borstein said. “They clean the bone, cut it a,nd turn it into chips.”
Quality control is handled externally by an independent inspector. Borstein said one of the first products developed by the bank was tendons that do not require radiation.
“Until 2022, tendons were routinely irradiated to prevent infection,” he said. “But radiation damages tendon quality, especially for sports medicine. We changed the sterilization protocol to preserve mechanical properties while maintaining safety.”
Donated bones undergo processing for use in oral and maxillofacial surgery, orthopedics, plastic surgery and oncologic surgery. Depending on medical needs, the bone can be used in solid form or ground into powder or fibers.
Dr. David Rotem, head of orthopedics at Emek Medical Center, said donated bones and tendons are a critical tool, particularly in sports injury repair.
“Many surgeons prefer tissue from deceased donors over commercial products, which lose some biological properties during processing,” he said. “This is especially important for oncology patients.”
Di Segni said the long-term vision is personalized medicine, in which the body becomes its own source of replacement parts.
“Until then, every donated bone is scanned and processed so we know exactly which shape fits which patient,” she said. “We are the national bank for bones and tendons, the only place in Israel using natural bone rather than titanium. But our biggest limitation is the low number of donors.”
She attributed the shortage to a lack of public awareness and gaps in transplant coordination. Borstein echoed the call, noting that a single tissue donation can help up to 75 patients.
“Tissue donation is often overlooked compared to organ donation,” he said. “But it saves and improves countless lives.”