A recent international study has uncovered a troubling gap between formal rehabilitation and patients’ real-life recovery once they return home.
Published in late October in the Journal of Rehabilitation and Disability Studies, the research offers an inside look at what truly happens to trauma survivors after hospital discharge and suggests that many feel left on their own just when they need support the most.
The study, conducted between December 2024 and September 2025, draws on in-depth interviews with twenty-seven senior rehabilitation experts from countries including Canada, New Zealand and the United Kingdom. These clinicians worked with patients recovering from everything from car accidents to severe combat injuries. Their shared experience paints a picture of patients who may leave rehab with restored mobility, but not with restored lives.
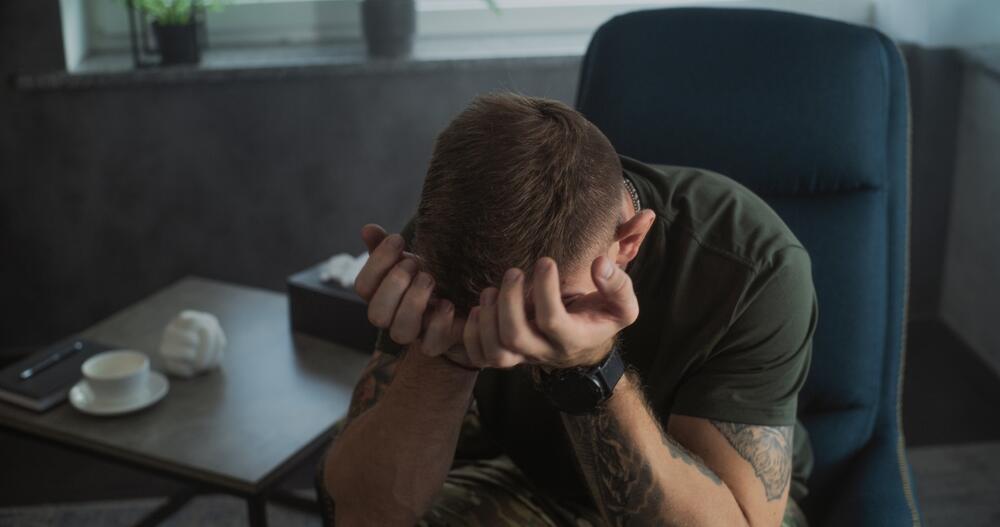
Lead researcher Dr. Louise McKenzie explains that, while the medical system often treats discharge as the end of care, patients experience it as the beginning of an uncertain and challenging new chapter. The study found that many struggle not only with lingering pain or mobility issues, but with emotional distress, a loss of identity and the overwhelming question of how to re-enter society in a meaningful way. Reintegration, whether social, emotional or professional, is rarely addressed in today’s medicalized model of rehabilitation.
Rehabilitation professionals interviewed in the study expressed a shared frustration: they are trained to heal the body, but often lack the tools or resources to support the person as a whole. Without a strong community network or coordinated long-term care, they say, patients are sent home “walking but not living.”
The findings resonate strongly in Israel, where trauma cases have surged over the past two years not only due to war-related injuries but also a rise in severe civilian trauma and chronic illness. The emotional and social dimensions of recovery are often overlooked, even though they are just as essential as physical healing.
“At our center, patients will finish rehab and look at us and say, ‘So what happens now?’” explains Shauli Hertzick Paz, CEO of the integrative rehabilitation center Medical Care. “The stitches and scars fade, but the sense of ‘becoming myself again’ can take months or even years. And that process requires more than physiotherapy. It requires a full team medicine, psychology, occupational therapy, cognitive support and family involvement. Real recovery happens not when the injury disappears, but when the person regains connection, purpose and identity.”
While the study does not claim to offer a single solution, it does make one thing clear: successful rehabilitation cannot be measured solely by range of motion or medical charts. It must include a person’s ability to return to life not just as a survivor, but as a whole and active human being.
- Shauli Hertzick Paz is the CEO of the integrative rehabilitation center - Medical Care. He manages hospitals and healthcare systems, a multidisciplinary therapist and the founder of the InHeal treatment method, which combines protocols for treating medical and emotional trauma