Israel's response to the rapid spread of the Omicron variant of COVID-19 has been chaotic to say the least, even the government managed to hold off its onset by imposing early restrictions on international travel.
In a special investigation conducted by Ynet, it emerged the government ultimately failed to use the extra time to prepare the health system, the economy and the education system for the eventual mass onslaugh
From the procurement of the Pfizer and Merc drugs to treat the virus and the roll out of a fourth vaccine – with its questionable efficacy - Israel is struggling with the surge in infections and the expected rise of hospitalizations.
Hospitals fear overcapacity
There has been no increase in hospital beds, including in intensive care units, since the first case of Omicron was detected in the country back late in November.
Health Minister Nitzan Horowitz told hospital administrators the Finance Ministry persists in its refusal to fund additional beds to treat COVID patients, while coronavirus czar Prof. Salman Zarka said beds were needed but could not specify how many.
5 View gallery


Medical staff treating a coronavirus patient at the Sheba Medical Center last week
(Photo: Yariv Katz)
The healthcare system in the community, meanwhile, is overburdened and unprepared, even though it is at the forefront of the Omicron wave. Israel's health maintenance organizations provide vaccines to the public and are responsible for most coronavirus testing, in addition to offering regular care to the population.
Despite being provided with additional manpower for vaccine drives, there has not been a comprehensive plan put in place to offer the resources needed to meet the demands of the pandemic. HMOs, therefore, appear to be on their own in this fight.
Health teams buckling under the load
As published on Ynet earlier this week, the Health Ministry was considering a change in policy that would allow healthcare workers, including doctors and nurses, to continue working while infected with coronavirus if they are asymptomatic.
This option came under attack from health experts and many others due to its lack of scientific wisdom. It proves just how severe the shortage in trained health professionals in medical centers and health funds is.
5 View gallery


Medical staff in the coronavirus ward at the Rabin Medical Center
(Photo: Rabin Medical Center PR)
Doctors and nurses are increasingly forced into quarantine, and hospitals fear they would be forced to close down medical wards and outpatient clinics due to lack of staff. For instance, Barzilai Medical Center in Ashkelon has already begun canceling scheduled elective surgeries.
In the meantime, additional staffing that was provided during earlier waves of the pandemic has not been provided during the Omicron wave.
The COVID testing debacle
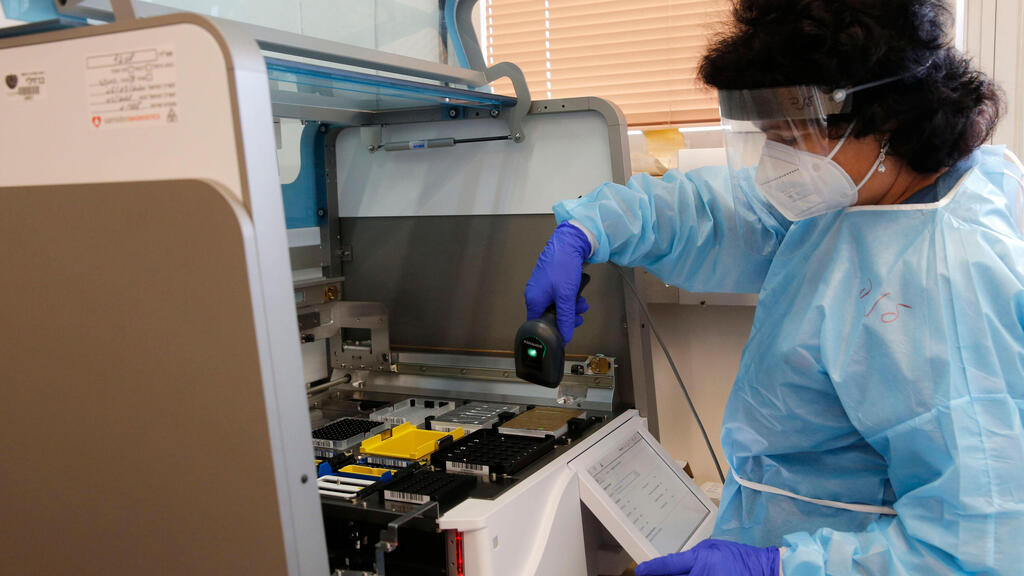
Rapid coronavirus tests, such as antigen, have proven to be unreliable, returning a false negative result in many of the cases. The IDF unit attached to the Health Ministry as a tool to help fight the pandemic, has warned in a press briefing that there has been no advanced preparation to increase lab capacity to deal with the massive amounts of the more reliable PCR tests being received for deciphering.
Despite the fact that Omicron is extremely contagious, as is evident by record-breaking number of single-day COVID cases, the labs are still only equipped to examine 170,000 PCR tests within a 24 hour period.
Delaying results could cause doctors to miss the opportunity to treat patients with the available drugs that must be given to COVID patients who are at risk of developing a severe illness from the virus.
Confusing government policies
Israelis wake up daily, wondering what changes to government policies will be announced today, creating nothing but constant confusion and undermining public's trust.
Last Thursday, we learned from the Health Ministry of a plan to test for COVID in schools, while the Education Ministry was not informed on it and in fact, refused to agree to such a plan.
Total chaos in the education system
Since the start of the Omicron wave, the education system became the poster child for chaos, with schools dealing with daily policy changes announced by the Education Ministry at the last minute.
Despite schools officially remaining open, thousands of students have once again been sent to study remotely due to exposure to virus carriers at schools across Israel.
This is perhaps the worst crisis faced by Israel's education system ever, effecting parents of schoolchildren all over the country, who don't know from one moment to the next whether their child will be at school tomorrow or if they will have to take a day off work.
In addition, after the Knesset Education Committee ended the designation of cities according to morbidity rates, schools found they had no guidelines in place to move forward.
Most classrooms contain around 30 students, crowded together in close quarters with most of them not having been vaccinated. Schools, therefore, were seen as the most likely place for infection. because no plan to divide kids into smaller study groups or capsules was devised.
School administrators, meanwhile, are made to solve staffing changes from one moment to the next and are operating with uncertainty, with teachers running back and forth between the children who were in class and those who were at home and needed instruction remotely.